Written by Taylor Woosley, Staff Writer. Unvaccinated subjects experienced a threefold mortality increase compared to vaccinated participants when serum 25(OH)D was less than 30 nmol/L.
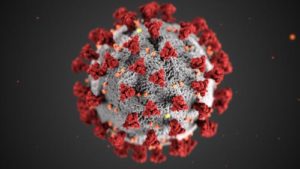 SARS-CoV-2, the novel coronavirus, causes the serious COVID-19 disease, a highly contagious and wide spreading disease associated with high morbidity and mortality1. COVID-19 infects pulmonary epithelial cells using the angiotensin converting enzyme-2 (ACE-2) receptors2. This induces an inflammatory state, evidenced by raised acute markers like interleukin-6 (IL-6), c-reactive protein (CRP), ferritin, etc. and may lead to lung damage relating to a cytokine storm3.
SARS-CoV-2, the novel coronavirus, causes the serious COVID-19 disease, a highly contagious and wide spreading disease associated with high morbidity and mortality1. COVID-19 infects pulmonary epithelial cells using the angiotensin converting enzyme-2 (ACE-2) receptors2. This induces an inflammatory state, evidenced by raised acute markers like interleukin-6 (IL-6), c-reactive protein (CRP), ferritin, etc. and may lead to lung damage relating to a cytokine storm3.
Several observational studies have shown a strong relationship between infection with COVID-19 and low serum levels of vitamin D4. Vitamin D exerts protective effects against acute respiratory tract infections through modulation of ACE-2 receptor activity, triggering the innate and adaptive immune responses, and reducing the levels of cytokines5. The innate immune system generates both pro-inflammatory and anti-inflammatory cytokines in response to viral and bacterial infections, and vitamin D can reduce the production of pro-inflammatory Th1 cytokines, such as tumor necrosis factor α6.
Sanecka et al. conducted a prospective cohort study to assess whether clinical outcomes in hospitalized COVID-19 pneumonia subjects are affected by varying vitamin D statuses, and whether any different effects were noted between vaccinated and unvaccinated participants. 171 participants who tested positive for SARS-CoV-2 at the Connolly Hospital in Dublin between June 15 and December 2021 were included in the study. Participants were deemed vaccinated if they had received at least two doses of an EU-approved vaccine within 6 months of hospital admission. Subject inclusion consisted of a confirmed COVID-19 diagnosis on nasopharyngeal swab PCR analysis, proof of vaccination status, and serum 25(OH)D levels measured at admission.
Information on age, sex, body mass index (BMI), smoking and alcohol status, comorbidities, oxygen requirement, mechanical ventilation, intensive care unit admission, and mortality were recoded and used in the analysis. One-tailed independent samples t-tests were utilized for normally distributed continuous variables to compare means (age, 25(OH)D) between binary groups with differing clinical outcomes. Of the 171 participants, the vaccinated subjects (n = 80) (average age of 69 years) were significantly older than unvaccinated participants (n = 91) (average age of 46 years) (p < 0.001). Average number of comorbidities in vaccinated subjects was 2.68, while unvaccinated subjects was 0.68 (p < 0.001). Significant findings of the prospective cohort study are as follows:
- Unvaccinated participants who needed prolonged supplemental oxygen had significantly lower vitamin D levels compared to vaccinated subjects and those requiring supplemental oxygen (p = 0.002, 95% CI 6.214-25.5).
- Among unvaccinated subjects, those in the ICU had significantly lower 25(OH)D levels compared to those not admitted to the ICU (p = 0.033, 95% CI -0.83-24.51).
- Greater age and lower mean serum 25(OH)D were observed in unvaccinated participants who died compared to those who survived (p = 0.005 and p = 0.049, respectively).
Results of the study suggest that advanced age was the main indicator of disease outcome in vaccinated participants, while in unvaccinated subjects both older age and low vitamin D status increased the risk of mortality. Sufficient vitamin D levels may provide immunological benefits for participants with COVID-19 infection.
Source: Sanecka, Martyna, Modar Youssef, Mohammad Abdulsalam, Syed F. Raza, Abdul Qadeer, Julia Ioana, Alya Aldoresi et al. “Hospital Outcomes in Patients Hospitalized for COVID-19 Pneumonia: The Effect of SARS-CoV-2 Vaccination and Vitamin D Status.” Nutrients 15, no. 13 (2023): 2976.
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Click here to read the full text study.
Posted September 12, 2023.
Taylor Woosley studied biology at Purdue University before becoming a 2016 graduate of Columbia College Chicago with a major in Writing. She currently resides in Glen Ellyn, IL.
References:
- Farid N, Rola N, Koch EAT, Nakhoul N. Active vitamin D supplementation and COVID-19 infections: review. Ir J Med Sci. Nov 2021;190(4):1271-1274. doi:10.1007/s11845-020-02452-8
- Mohan M, Cherian JJ, Sharma A. Exploring links between vitamin D deficiency and COVID-19. PLoS pathogens. Sep 2020;16(9):e1008874. doi:10.1371/journal.ppat.1008874
- Rawat D, Roy A, Maitra S, Shankar V, Khanna P, Baidya DK. “Vitamin D supplementation and COVID-19 treatment: A systematic review and meta-analysis”. Diabetes & metabolic syndrome. Jul-Aug 2021;15(4):102189. doi:10.1016/j.dsx.2021.102189
- Gibbons JB, Norton EC, McCullough JS, et al. Association between vitamin D supplementation and COVID-19 infection and mortality. Sci Rep. Nov 12 2022;12(1):19397. doi:10.1038/s41598-022-24053-4
- Shah K, Varna VP, Sharma U, Mavalankar D. Does vitamin D supplementation reduce COVID-19 severity?: a systematic review. Qjm. Oct 25 2022;115(10):665-672. doi:10.1093/qjmed/hcac040
- Grant WB, Lahore H, McDonnell SL, et al. Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients. Apr 2 2020;12(4)doi:10.3390/nu12040988
